Report on first successful human gene therapy, DRCC Paris, June 2001
Gene therapy: Safer and Virus Free, Science News Focus, 23 Nov. 2001
Stem cell based gene therapy of ADA-SCID, Science 28 June 2002
Success with unclear risk, Science News, 18 Oct. 2002
Second Child in French Trial found to have leukemia, Science News, 17 Jan. 2003
New York Times Report on 2nd leukemia victim linked to gene therapy protocol, Jan. 2003
Gene therapy halt, New York Times, Jan. 2003
Gene therapy Insertional Mutagenesis Insights, Science 2004
Third Child gets Cancer, SCIDs trial halted again, Nature 2005
Restarting Gene Therapy Trials, Nature 2005
Immunodeficiencies: Injecting some safety into SCID gene therapy?, Nature 2006
Second Coming of Gene Therapy: Discover 2009
Gene Therapy of Human Severe Combined Immunodeficiency (SCID-XI) Disease
The potential for gene therapy to cure human diseases has been around for 20 years. Many trials--- no successes. The main problem has been figuring out how to target a normal transgene (or repair the endogenous defective gene) to the right somatic cells.
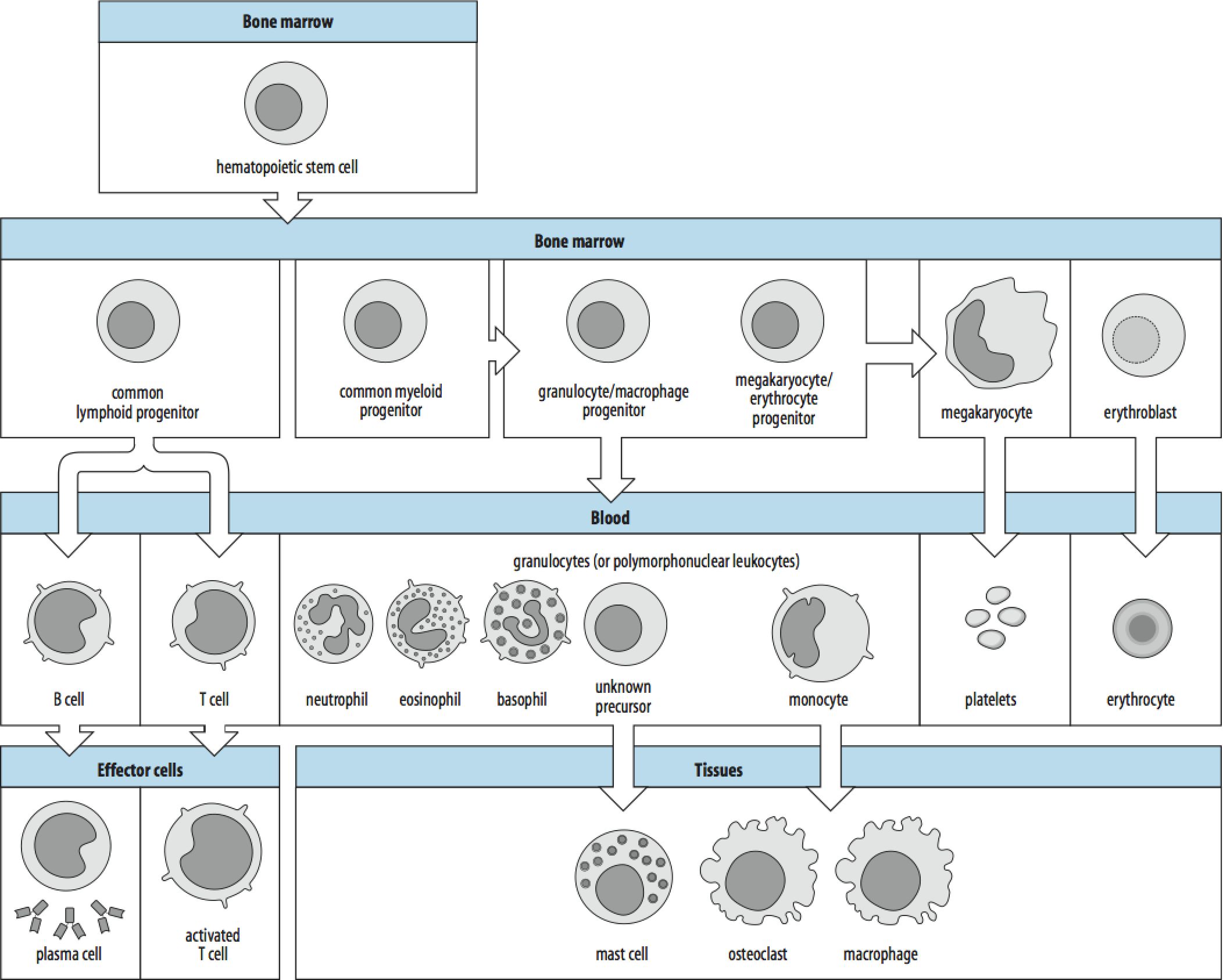
Gene deficit in gamma c cytokine receptor subunit of Interleukin 2, 4, 7, 9 and 15 receptors. This gene is expressed in immune (blood) stem cells and stimulates proliferation and differentiation to produce T and NK Lymphocytes.
SCID-X1 children have No T and NK Lymphocytes!
No protection against viral or bacterial infection. This is generally lethal and gives rise to the "Bubble boy” – children who must live completely isolated from any source of viral or bacterial infections. Only successful long term treatment is bone marrow transplantation IF suitable donor can be found.
This inherited disease is a well understood genetic defect in single gene causing serious disease: Excellent model to test gene therapy. There was good evidence that gene therapy would work.
Spontaneous reversion of mutation in one child – normal gama c gene in small population of stem cells cured disease even though there was a large population mutant cells.
This strongly suggested that stem cells normally expressing gamma c have a selective advantage, ie., binding of ligand stimulates production of enough T and NK lymphocytes to give relatively normal immune response.
Early in 2000, two children with SCID-XI who could not get bone marrow transplants were chosen as first candidates for gene therapy. They were 8 and 11 months old.
Protocol
1. Harvest marrow cells from child (107-108 cells).
2. Grow in laboratory culture and infect with retroviral vector containing normal gamma c gene. Retroviral vector will infect cells and randomly insert gamma c gene into genome.
Scientist hoping for insertion into T and NK Lymphocyte stem cells – and normal expression.
Scientists are relying on the selective advantage of stem cells expressing normal gamma c (increased replication and production of T and NK lymphocytes).
3. Re-inject transfected cells into child.
It Worked!
3 months later the children had normal levels of T and NK lymphocytes and a normal immune response to viral and bacterial challenge.
Children went home and showed normal development and a normal immune funtion.
Everyone was euphoric!!! 9 more children were treated with the same same protocol.
2 major UNKNOWNS.
1. Permanent cure? It wasn't known which stem cells were targeted--- immortal or short lived.
2. Will transgene remain active?
For unknown reasons many transgenes are unstable over time.
2 years later----Disaster
September 2, 2002
1st child develops leukemia (fluke? Other children in family had early cancers)
Then 4 months later 2nd child leukemia
Most retroviral gene therapy trials halted.
What Happened?
Other trials using retroviral vectors had suggested they were safe, even though all knew of the probability of random insertion that would activate an oncogene. The development of cancer usually requires a multi-step process involving activation of multiple oncogenes. It was thought there was very low probability of a single insertion activation and oncogene and causing cancer.
They sequenced the insertion site in the two children that developed leukemia. Both transgenes had landed near the LMO-2 gene -----a known oncogene involved in some childhood leukemias. Too much of a coincidence to ignore.
How Possible?
Probability ~ 1 in 100,000 that retrovirus will randomly insert near enough to LMO-2 to activate.
But 107-108 cells transfected – given transfection efficiency, this means each child probably received several cells with transgenes near LMO02!
Still activation of any one oncogene should not produce leukeumia.
Now thought that gamma c cytokine receptor gene itself is slightly oncogenic.
We know it gives cells a selective growth advantage and stimulates replication.
Bad Luck –
Future :identify and grow stem cells in lab
: targeted gene replacement
Update from Scientific Group that initiated the SCIDs Gene therapy trial. They have continued treated children and have improved safety and long term success.
Editorial
Molecular Therapy (2010) 18 11, 1891. doi:10.1038/mt.2010.228
Gene Therapy for SCID-X1: Round 2
Roland W Herzog1
1Deputy Editor
When reported in 2000, gene therapy for X-linked severe combined immune deficiency (SCID-X1) represented a first clear success in clinical gene therapy, providing a tremendous boost for the field. Retroviral gene transfer of the common cytokine receptor γ-chain, required for the function of multiple cytokine receptors, to bone marrow–derived hematopoietic stem and progenitor cells reconstituted development of functional T cells and thereby also partially restored the ability of the affected boys to mount proper B-cell responses. Gene therapies were performed in two clinical trials in France and the United Kingdom in a total of 20 boys. However, the approach experienced a major setback when 5 of the 20 boys developed leukemia due to insertional mutagenesis and activation of an endogenous proto-oncogene. These events led to the development of highly sensitive polymerase chain reaction techniques to detect viral integration sites and improve vector design, thereby substantially increasing safety of clinical trials based on integrating vectors.
At the same time, during the period of continual attention to the leukemia cases, including by news media, the tremendous success achieved by these trials seemed almost unnoticed. The findings of long-term follow-up on nine boys from the French trial, now 8–11 years old, were recently published. One of the four children who developed leukemia in this trial had died. The other three were successfully treated with chemotherapy and were among seven children who exhibited long-term immune reconstitution. Gene-corrected T cells have persisted for more than 10 years. The seven children with functional immune systems have responded to vaccination and live fairly normal lives. Remarkably, four of the seven have not required immunoglobulin infusions although long-term transduction of B cells was not observed. The results from the London study show similar effects on restoration of immunity, and only one child has developed leukemia. In this regard, gene therapy appears to offer a genuine therapeutic alternative to mismatched allogeneic hematopoietic stem cell transplantation (HSCT).
When evaluating the success of gene therapy for SCID-X1, one must keep in mind that the disorder has very poor prognosis without treatment and results in death from infectious disease in the first year of life. SCID-X1 can be cured by HSCT. However, a matched family donor is available only for approximately 30% of patients. Transplants from unrelated or haploidentical donors are complicated by graft-versus-host disease (GvHD), side effects of chemotherapy, and incomplete lymphoid reconstitution. Gene therapy, using the patient’s own cells, avoids the need for matched donors as well as GvHD and other bone marrow transplant–related complications. An argument has arisen in the gene therapy field about the relative contributions of the transgene (which in SCID-X1 provides a substantial growth advantage over untransduced cells) and the vector. Murine gammaretroviral vectors have a tendency to integrate in the promoter region of transcriptionally active genes and, in the case of patients with SCID-X1, favored clonal dominance for cells with integration near, in particular, the T-cell oncogene Lmo2. Interestingly, gene therapy for ADA-SCID, using a similar gammaretroviral vector, was not plagued with leukemia, suggesting contributions by the vector and the specific disease/transgene to the malignancy.
In 2008, an article in Molecular Therapy (Mol Ther 16: 590−598) described a new generation of self-inactivating (SIN) vector that lacks all enhancer–promoter elements of the gammaretroviral LTR U3 region. Such a vector is less likely to activate nearby endogenous genes following integration into a host chromosome. Furthermore, expression of the IL-2RG gene in this vector is driven by a promoter element from the human elongation factor 1-α gene, thereby providing more physiological levels of transgene expression. On the basis of this vector, a multi-institutional phase I/II trial involving collaborators in the United States and Europe is now enrolling patients. The trial seeks to enroll a total of 20 boys who are at least 4 months old and lack a readily available matched bone marrow donor. Participating clinical sites in Europe include Great Ormond Street Hospital (London), Hôpital Necker (Paris), and, in the United States, Children’s Hospital Boston, Cincinnati Children’s Hospital Medical Center, and the University of California, Los Angeles. A promising treatment strategy now enters a second phase, hopefully leading to a cure for SCID-X1 with reduced risk for leukemia while avoiding the complications of traditional transplantation.
Check out this link to the Human Genome Project Information for "current" updates on gene therapy trials.
Other diseases?
Recent (2012) NYTs article on making artificial organs
Successful treatment of TB damaged windpipe
Building a new heart (This link will only work from U of U network)
Treating Stroke (This link will only work from U of U network)
First Stem Cell Trial in US (Time Magazine)
First Stem Cell Trial in US (NYT)